What is a mastectomy?
A mastectomy is surgery to remove the breast. It's often done as part of breast cancer treatment. It may also be done to prevent breast cancer. The type of mastectomy depends on the type and location of the cancer and your treatment plan. It also depends on whether you have breast reconstruction, and whether it's done at the same time as the mastectomy. Talk with your doctor about your surgery options and whether any lymph nodes will be removed.
Why is a mastectomy done?
Mastectomy is done to remove the breast. It's usually done to help treat or prevent breast cancer.
Breast surgery: Modified radical mastectomy
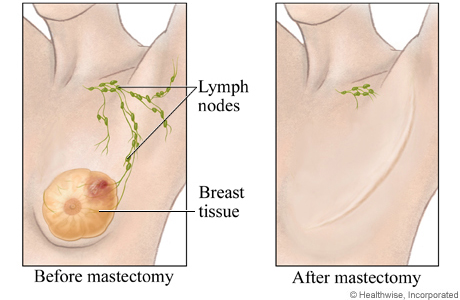
A modified radical mastectomy is the removal of the breast, the lymph nodes under the arm, and the lining over the chest muscles. This is a common type of surgery for breast cancer.
When should you call for help after a mastectomy?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have chest pain, are short of breath, or cough up blood.
Call your doctor now or seek immediate medical care if:
- You are sick to your stomach or cannot drink fluids.
- You cannot pass stools or gas.
- You have pain that does not get better after you take your pain medicine.
- You have loose stitches, or your incision comes open.
- Bright red blood has soaked through the bandage over your incision.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness or swelling in your leg.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have any problems.
- You have new or worse swelling or pain in your arm.
©2011-2025 Healthwise, Incorporated
