Scleral buckling surgery for retinal detachment: Overview
Scleral buckling surgery is a common way to treat retinal detachment. It is a method of closing breaks and flattening the retina.
A scleral buckle is a piece of silicone sponge, rubber, or semi-hard plastic that your eye doctor (ophthalmologist) places on the outside of the eye (the sclera, or the white of the eye). The material is sewn to the eye to keep it in place. The buckling element is usually left in place permanently.
The element pushes in, or "buckles," the sclera toward the middle of the eye. This buckling effect on the sclera relieves the pull (traction) on the retina, allowing the retinal tear to settle against the wall of the eye. The buckle effect may cover only the area behind the detachment, or it may encircle the eyeball like a ring.
By itself, the buckle does not prevent a retinal break from opening again. Usually extreme cold (cryopexy) or, less commonly, heat (diathermy) or light (laser photocoagulation) is used to scar the retina and hold it in place until a seal forms between the retina and the layer beneath it. The seal holds the layers of the eye together and keeps fluid from getting between them.
Other facts about the surgery
- The surgery takes place in an operating room, usually on an outpatient basis (you go home the same day).
- Local or general anesthesia may be used.
- Before the surgery, your eye doctor may patch both of your eyes and have you stay in bed to keep the detachment from spreading. Right before surgery, the doctor will use eyedrops to dilate your pupils and may trim your eyelashes to keep them out of the way.
- A first-time surgery usually lasts 1 to 2 hours. Repeat surgeries or more complex detachments may take longer.
Why is scleral buckling surgery for retinal detachment done?
Scleral buckling is effective in supporting a tear, hole, or break in the retina that has caused the detachment. It is rarely helpful on its own when scar tissue tugging on the retina has caused the detachment (traction detachment).
Scleral Buckling: After Surgery
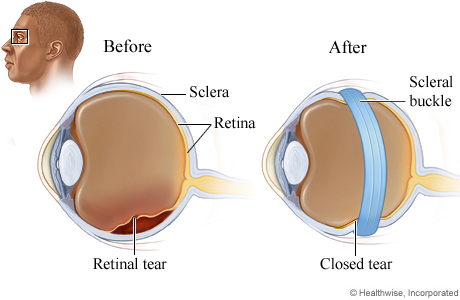
A scleral buckle is a piece of silicone sponge, rubber, or semi-hard plastic. In scleral buckling surgery, the buckle is placed against the outer surface of the eye and sewn onto the eye to keep it in place. The buckle pushes the sclera toward the middle of the eye, relieving the pull on the retina and allowing the tear to settle against the wall of the eye.
Extreme cold (cryopexy) or light (laser photocoagulation) is used to scar the area around the tear. The scarring helps keep this area from moving so that a seal can form between the retina and the layer beneath it. In most cases, the buckle will stay on the eye forever.
How well does scleral buckling surgery for retinal detachment work?
Placing a scleral buckle reattaches the retina in most cases.
Chances for good vision after surgery are higher if the macula was still attached before surgery. If the detachment affected the macula, good vision after surgery is still possible but less likely.
©2011-2025 Healthwise, Incorporated
